Engineers from Northwestern University in Illinois, United States, have developed a pacemaker so small that it can be implanted in the body non-invasively using a syringe. Although its creators indicate that it can function in hearts of all sizes, it seems that this new device is especially suitable for newborns with congenital heart defects, with small and fragile hearts.
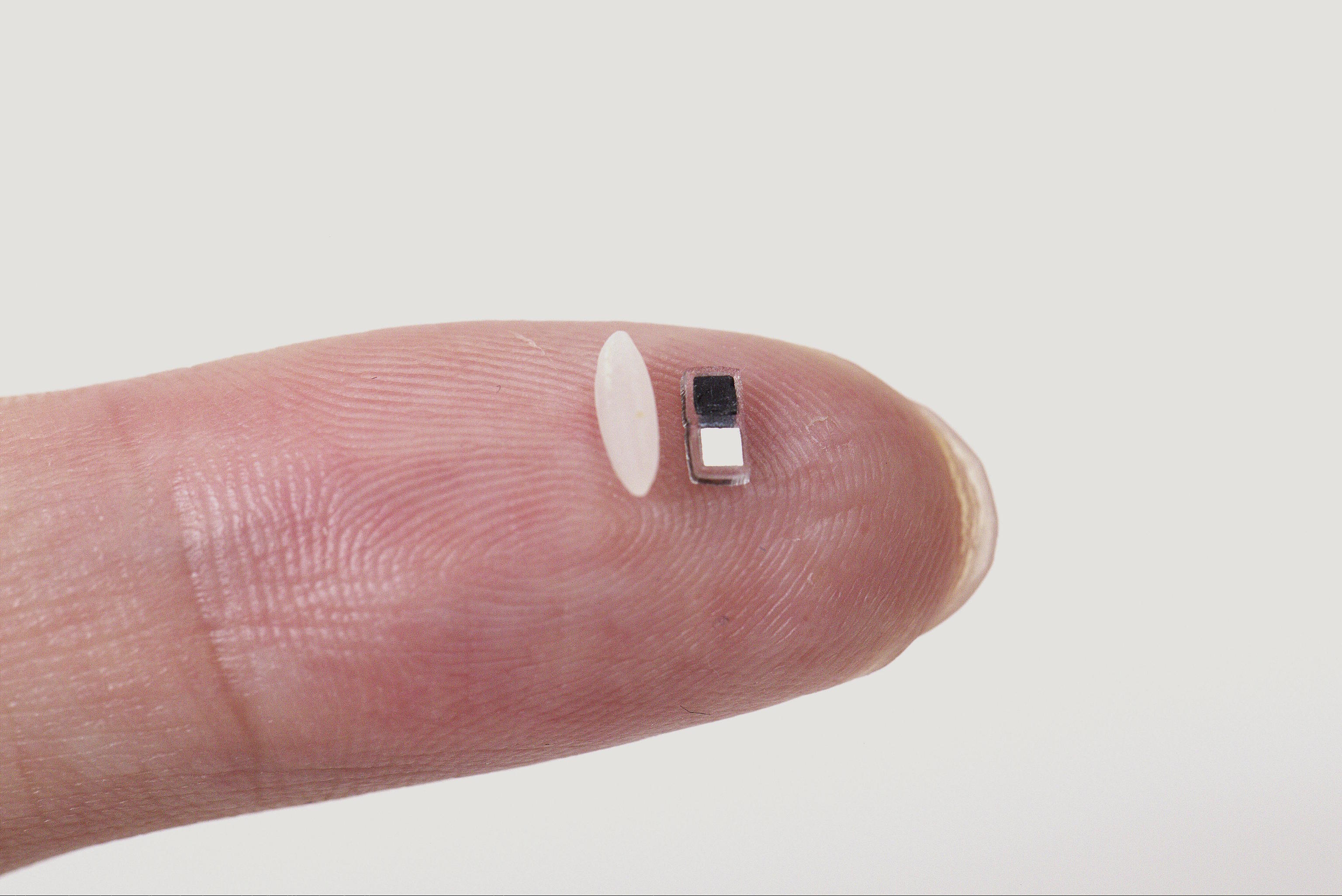
Smaller than a grain of rice, making it the current smallest pacemaker in the world, it attaches to a small, portable, soft, flexible, and wireless device placed on the patient's chest to control stimulation. When the portable device detects an irregular heartbeat, it automatically emits a light pulse to activate the pacemaker, so it is light-activated. These short pulses, which penetrate the patient's skin, sternum, and muscles, control stimulation.
Designed for patients who only need a temporary device, the pacemaker easily dissolves when no longer needed. All its components are biocompatible, so they dissolve naturally in bodily fluids, avoiding the need for surgical extraction, as explained by the researchers in Nature.
The work also demonstrates the effectiveness of the device in a series of large and small animal models, as well as in human hearts from deceased donors. This development follows the trend of recent years in achieving smaller devices that allow less invasive implantations, benefiting patients, especially pediatric ones.
John A. Rogers, a pioneer in Bioelectronics at Northwestern and director of the device's development, points out that "as far as we know, it is the smallest pacemaker in the world. There is a crucial need for temporary pacemakers in the context of pediatric heart surgeries. This is an example of use where size miniaturization is essential. Regarding the device's burden on the body, the smaller, the better."
Although the pacemaker is very small (measuring just 1.8 millimeters wide, 3.5 millimeters long, and 1 millimeter thick), it provides as much stimulation as a full-size pacemaker.
According to Igor Efimov, an experimental cardiologist at Northwestern and co-director of the work, children have been the main motivation for developing this new device, considering that around 1% of children are born worldwide with congenital heart defects, regardless of whether they live in resource-rich or resource-poor countries.
"The good news is that these children only need a temporary pacemaker after surgery. In about seven days, most patients' hearts will self-repair. But those seven days are crucial. Now we can place this tiny pacemaker in a child's heart and stimulate it with a soft, delicate, portable device. And no additional surgery is required to remove it," explains this professional regarding this new device, in the development of which Yonggang Huang, a professor of Mechanical and Civil and Environmental Engineering, Marcia Achenbach, as well as Wei Ouyang, a professor of Engineering at Dartmouth College; and Rishi Arora, a Medicine professor at the University of Chicago, have also participated.
Meeting an unmet clinical need
This work culminates a previous collaboration between Rogers and Efimov, in which they developed the first absorbable device for temporary pacemakers. Many patients need temporary pacemakers after heart surgery, either while waiting for a permanent pacemaker or to help restore a normal heart rate during recovery.
Currently, surgeons sew the electrodes to the heart muscle during the procedure. The electrode wires exit through the front of the patient's chest, where they connect to an external pacemaker that supplies a current to control the heart rhythm. When the temporary pacemaker is no longer needed, doctors remove its electrodes. Possible complications include infection, detachment, tearing or tissue damage, bleeding, and blood clots.
Efimov explains that "the wires protrude from the body, connected to an external pacemaker. When the pacemaker is no longer needed, the doctor removes it. The wires can become wrapped in scar tissue. Therefore, when removed, they can damage the heart muscle. This is how American astronaut Neil Armstrong died. He had a temporary pacemaker after bypass surgery. When the wires were removed, he suffered internal bleeding," recalls the researcher.
In response to this clinical need, these teams developed a dissolvable pacemaker, presented in Nature Biotechnology in 2021. A thin, flexible, and lightweight device that eliminated the need for bulky batteries and rigid hardware, including wires. Rogers' laboratory was the inventor of the concept of bioresorbable electronic medicine: electronic devices that provide therapeutic benefit to the patient and then dissolve in the body without causing harm, like absorbable sutures. By varying the composition and thickness of these devices' materials, the team can precisely control the number of days they remain functional before dissolving.
Steps towards miniaturized devices
"Our original pacemaker worked well," says Rogers. "It was thin, flexible, and fully absorbable. But the size of its receiving antenna limited our ability to miniaturize it. Instead of using the radiofrequency scheme for wireless control, we developed a light-based scheme to power the pacemaker and deliver stimulation pulses to the heart's surface. This feature allowed us to drastically reduce its size."
To further reduce the device's size, the researchers also reimagined its power source. Instead of using near-field communication (NFC) to supply power, the new tiny pacemaker operates using a galvanic cell, a type of simple battery that converts chemical energy into electrical energy. Specifically, the pacemaker uses two different metals as electrodes to deliver electrical pulses to the heart. Upon contact with surrounding biofluids, the electrodes form a battery. The resulting chemical reactions cause electric current to flow to stimulate the heart.
Integration with other implantables
The team has used an infrared light wavelength that penetrates deeply and safely into the body. If the patient's heart rate drops below a certain level, the portable device detects the event and automatically activates a light-emitting diode. The light flashes at a frequency similar to the normal heart rate.
Efimov explains that "the heart requires minimal electrical stimulation. By minimizing the size, we drastically simplify implantation procedures, reduce trauma and risk for the patient, and, thanks to the device's soluble nature, eliminate the need for secondary surgical extractions."
According to the article, it would also be possible to place several of these small pacemakers on the heart's outer surface, achieving better synchronized functional care. "We could also incorporate our pacemakers into other medical devices, such as heart valve replacements, which can cause heart blockage," according to the authors.
Rogers emphasizes that due to its small size, this pacemaker can be integrated with virtually any type of implantable device. The study data demonstrate the integration of sets of these devices into structures that serve as transcatheter aortic valve replacements.
The versatility of technology opens up a wide range of other possibilities for use in bioelectronic medicines, including helping to repair nerves and bones, treat wounds, and block pain.
In Spain, according to Julián Pérez-Villacastín, head of the Cardiology Department at the Hospital Clínico San Carlos in Madrid and former president of the Spanish Society of Cardiology (SEC), more than 40,000 pacemakers are implanted every year. "These devices are used to prevent the heart from stopping in people with abnormalities in the electrical system of their heart," he points out. Their size has been progressively reduced, and there are even current pacemakers that "do not require wires and are implanted directly inside the heart. But all of them carry risks and still need to be replaced when their battery expires."
This work presents, according to the cardiologist, an exceptional prototype. First, because "it is a miniature, which can be transported using catheters until it is implanted in the heart walls. Also, because the way in which the electrical impulses are generated is absolutely original. This opens up the possibility of implanting several devices that stimulate the heart simultaneously, increasing the efficiency of contraction."
Although he considers it spectacular, he insists that "it is an experimental prototype. The idea is brilliant, but it will take years for this technology to be able to be implanted in humans with sufficient guarantees." He details that the prototype presented "only allows for temporary stimulation, which could be useful for patients who require a pacemaker for a very short period. This is not the norm, because the norm is that people who need a pacemaker need it for life. However, he does not diminish the importance of these developments that mark how fascinating future medicine will be."