From a daily pill for pre-exposure prophylaxis, known as PrEP, to an injection every six months, "it is a giant step in the field of HIV prevention," experts say. The US Food and Drug Administration (FDA) has approved a new treatment to prevent HIV, as announced by the pharmaceutical company Gilead, which developed it.
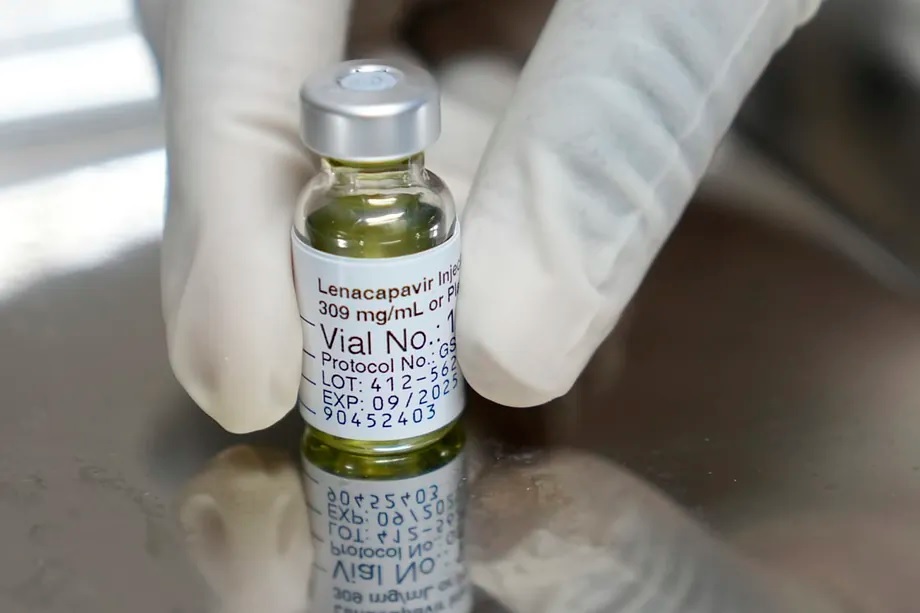
The active ingredient in this treatment is lenacapavir and consists of two annual injections. "It is a treatment that inactivates the virus," explains Alfonso Cabello, a specialist in Internal Medicine and Infectious Diseases at the Jiménez Díaz Foundation. At the same time, he details that, following the scientific endorsement from the US, "now we need to know how it will be implemented."
The FDA based its decision on the high demonstrated effectiveness in preventing infections: over 96%. Two studies, called Purpose 1 and 2, have measured the efficacy of using the injectable in over 8,000 people worldwide. On one hand, it has been shown to provide a 100% shield against infection in cisgender women in Africa. On the other hand, it has demonstrated protection for cisgender men and gender-diverse individuals of up to 96%.
The results that paved the way for their submission to regulatory agencies were communicated in September 2024. "From a long-term prevention perspective, we are facing a form of prevention that resembles a seasonal vaccine," says Cabello.
At that time, based on the communicated results, the independent Data Monitoring Committee (DMC) recommended that Gilead, the company responsible for the molecule, stop the blind phase of the Purpose 1 trial and offer open-label lenacapavir to all participants. The research involved over 5,300 cisgender women and adolescents aged between 16 and 25 in 25 sites in South Africa and three sites in Uganda.
In Purpose 2, the same regimen of daily pill and injection every six months was also compared. In this case, it involved 2,180 participants who were cisgender men, transgender men, transgender women, and non-binary individuals in Argentina, Brazil, Mexico, Peru, South Africa, Thailand, and the United States who have sex with partners assigned male at birth.
It is a drug that has demonstrated safety, but also "good tolerability." "The only thing people report is pain at the intramuscular injection site for a while," explains Cabello.
A key advance in eliminating HIV transmissions
The magnitude of the advance against HIV was recently highlighted by the journal Science. Containing the spread of infections when used in at-risk individuals as pre-exposure prophylaxis was recognized as the discovery of the year in 2024.
Still under investigation is what could be considered the first HIV vaccine. "Pharmacokinetic data from a single injection at one year have been presented. They are preliminary data, but very promising," says Cabello. In March, the research was simultaneously presented at the Conference on Retroviruses and Opportunistic Infections (CROI) and in the journal The Lancet.
In this phase 1 trial, 40 HIV-negative participants aged between 18 and 55 were injected with one of the two lenacapavir formulations administered as a single dose. Samples were collected at pre-specified time points up to 56 weeks to evaluate the safety and pharmacokinetics of the injection. Overall, the medication was well tolerated, with injection site pain being the most common adverse event.
Enhancing the shield against HIV with a molecule against the most resistant forms
Medications aimed at preventing HIV transmission have existed for over a decade, based on taking a daily pill. "Therapeutic compliance poses complications in controlling and preventing transmission," says Cabello. The specialist argues that "there are social determinants that can complicate adherence."
Since 2022, this molecule has been available in the form of antiretroviral treatment "for the most resistant forms, that is, in those infections where other medications do not have the desired effects on patients," notes Cabello. Marketed in Spain as Sunleca, it has been funded by the Health Ministry in our country for almost a year.
The administration method is the same as for prophylaxis: twice a year subcutaneously. Around 250 complex patients who did not respond to up to four drug families benefit from it. In patients with multi-resistant HIV, the medication, in combination with an optimized baseline treatment, demonstrated in the Capella clinical trial that led to approval, an 83% efficacy in terms of virological suppression.
Obstacle: high prices
Although the company has not disclosed them, analysts estimate that the launch price in the US could reach $25,000 per year. For this reason, many have called on the laboratory to make these treatments accessible in poor countries, for example, by allowing generics to be manufactured.
Gilead maintains, as it assures this medium, that it is committed to achieving broad and sustainable access to lenacapavir for PrEP in high-incidence, resource-limited countries, which are mainly low- and lower-middle-income countries. In anticipation of possible approval by regulatory agencies of the injectable for PrEP, the laboratory is working on a dual access strategy: on one hand, developing a robust program of direct voluntary licenses to accelerate access to generic versions of lenacapavir in high-incidence, resource-limited countries; and, on the other hand, supplying the molecule at no profit to the company to countries included in the voluntary license agreements until generic manufacturers can fully meet demand.
"Gilead has included a total of 120 countries in its voluntary licensing agreements based on a thoughtful and rigorous process that prioritizes speed and tailors approaches to each country and region," the company states. Criteria such as "unmet needs, therapeutic area, economic situation (based on World Bank classifications to identify income levels of countries), economic inequality within the country, disease burden, and the ability to reach patients" have been taken into account.